What is it ?
Low back pain is defined as pain in the lumbosacral area, most often due to natural aging of the spine: wear of the disc (degeneration, disc disease etc.), and of the facet joints. Low back pain is frequently referred to as “acute” or “chronic”.
In reality, everyone suffers from low back pain at some point in life. A small proportion of patients will keep constant, but bearable, lower back pain, which will be referred to as “chronic” with sometimes severe pain reducing the daily, social and professional capacities, for a more or less long period (days, sometimes weeks).
These painful attacks can most often occur spontaneously or in relation with certain strenuous physical activity. The frequency of these acute pain phases can be limited by regular practicing of strengthening exercises (sheathing, Pilates, etc.) or sports activities.
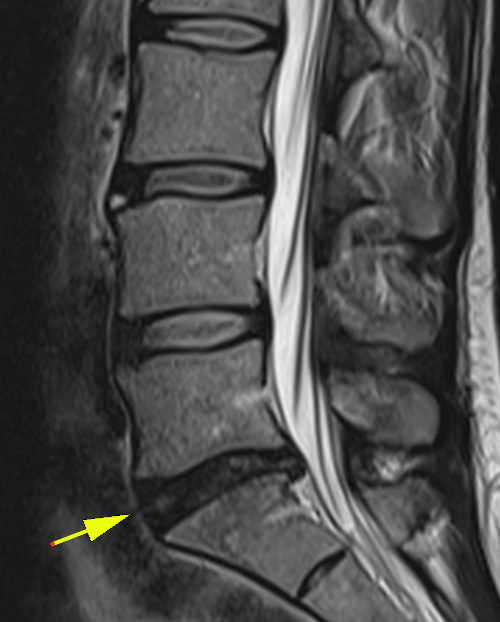
Below, an MRI image of degeneration (natural wear) of the L5-S1 disc (yellow arrow). It should be noted that this is only a radiological image, whose clinical manifestations, again, are very variable: many people with such disks do not suffer pain!