What is it ?
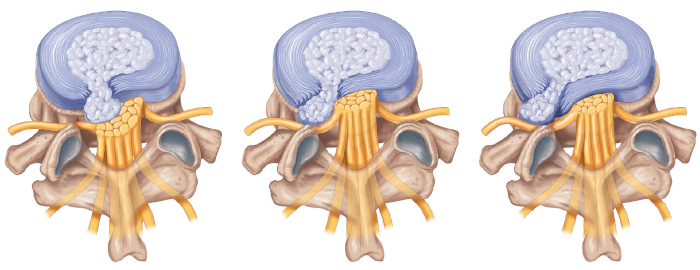
Lumbar disc herniation is a consequence of degeneration (normal aging) of the lumbar intervertebral disc. Part of the disc may protrude back into the lumbar vertebral canal, through which the nerve roots of the lower limbs travel. Below: a drawing representing three different types of lumbar disc herniation. We can see the fibrous annulus (in blue) through which a fragment of the disc nucleus has extruded.