What is it ?
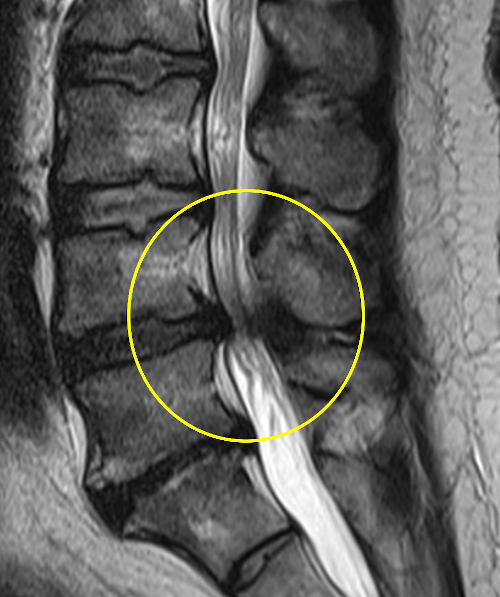
Lumbar spinal stenosis also results from disc degeneration. This causes a transfer of mechanical charges on the articular facets in particular, producing in the long term osteophytary beaks (bony outgrowths) encroaching into the lumbar canal. The volume available for the nerve roots is thus reduced. Most often it is patients over 50 who are affected. The MRI image below shows a narrowing of the L4-L5 level (yellow circle).