What is it ?
It is a three-dimensional deformity of the spine, usually in the thoracic or lumbar region, or across the two anatomical regions.

It is a three-dimensional deformity of the spine, usually in the thoracic or lumbar region, or across the two anatomical regions.

There are various types of scoliosis. The most common are adolescent idiopathic scoliosis in children, and degenerative scoliosis in adults.
Scoliosis of the adolescent is asymptomatic (no pain), which makes diagnosis sometimes difficult. Girls are more likely to develop scoliosis at the time of the growth peak (between 11 and 13 years, boys less often and between 13 and 15 years). In Europe, there is a systematic screening in schools. Sometimes children or parents notice an asymmetry of the waist or the shoulder height.
In adults, scoliosis is more frequently painful. It is either due to progression of a deformity that was present since adolescence (idiopathic scoliosis), or the development of a new scoliosis due to degenerative alterations of the spine (de novo degenerative scoliosis). The pain can be either low back pain or radicular pain or neurogenic claudication (see lumbar spinal stenosis).
Your doctor will ask for a specialized advice based on your symptoms. If it is common low back pain, the treatment will be nonsurgical. If the pain is disabling and affects the quality of social and professional life, or if there are neurological symptoms, a surgical opinion may be necessary.
In adolescents, the treatment will aim to prevent the progression of scoliosis. A radiological follow-up will be necessary according to the potential of progression of the deformity, which depends on the severity of the deformity and the residual growth estimate at the time of the diagnosis. Treatment will include physiotherapy, or a brace or both.
In adults, we will treat pain, using medication, muscle strengthening and posture exercises, physiotherapy, osteopathy, and so on. Sometimes spinal injections may be attempted.
In adolescents, surgical treatment is indicated in case of severe deformity (criteria vary according to the anatomical location of scoliosis), or risk of progression, which depends on residual growth potential. The goal is to avoid pain or cardiopulmonary complications in adulthood (progression of thoracic scoliosis reduces the volume available for the heart and lungs).
In adults, surgical treatment is indicated not only to prevent progression of the deformity, but also, and more often, to reduce painful symptoms: disabling low back pain or lumbar spinal stenosis symptoms.
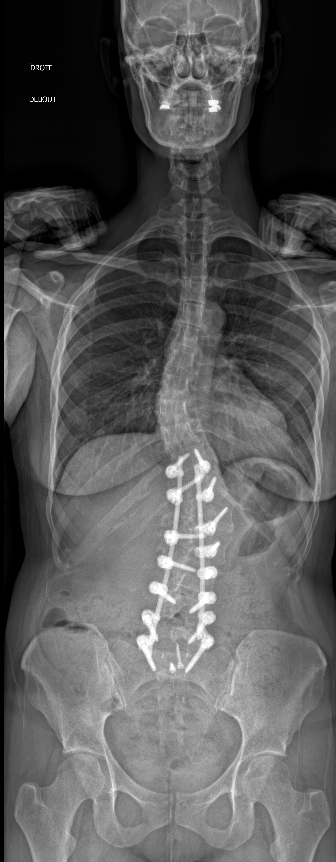
Adult scoliosis surgery involves more or less invasive treatments depending on the type and severity of the deformity. The most frequently used technique involves a posterior surgical approach and the placement of implants (screws and rods) that will be used to correct and maintain this correction. Bone grafting is necessary to sustain the fusion in the long term.
Less invasive techniques can be used in adolescents because their deformity is usually less rigid, and therefore easier to reduce.
In adults, rehabilitation starts the day after surgery. Daily life activities are resumed as soon as possible within the limit of pain. Walking is mainly recommended for the first 6-8 weeks after surgery, then gradual increase of activities, including sports, are allowed.
Serious complications are low (<5%, and severe neurological complications close to 0%). In patients over 60 years of age, and depending on the general health status, there might be mechanical complications related to osteopenia/osteoporosis. This type of surgery must be performed by an experienced team of surgeons and anesthesiologists, such as those from the Geneva Back Center. Your surgeon will give you detailed explanations about the surgical procedure during the preoperative interview.